The National Academy of Medicine (NAM) recently published a significant document that I am recommending to every CIO/CTO in healthcare as well as informing what I do as a newly appointed commissioner on the State of Michigan Health IT Commission.
The paper was written by a thoughtful group of scientists, physicians, and leaders from John Hopkins, Emory, DoD, VA, Mass General, ONC, Anthem, NIST, and staff of the National Academy of Medicine.
As a CIO or CTO in healthcare, you know that one of the most challenging but necessary requirements in providing high-quality care is the interoperability between systems, technology, and data. It’s a problem that creates barriers to delivering patient outcomes and is not a simple one to solve.
The thesis of the NAM’s document is that the interoperability problem can be addressed by a commitment to standards and data mobility that transcend individual technology purchases and is made a primary value when contracting or acquiring healthcare technology. By raising interoperability as a primary piece of criteria for decision-making and contracting, provider organizations can use the power of the market to begin moving the needle of what has become a systemic issue in the US healthcare system.
We begin by recognizing that interoperability works at a variety of layers. The lower levels are easier to accomplish by technologists. The higher layers require significant process and people effort at the business level.
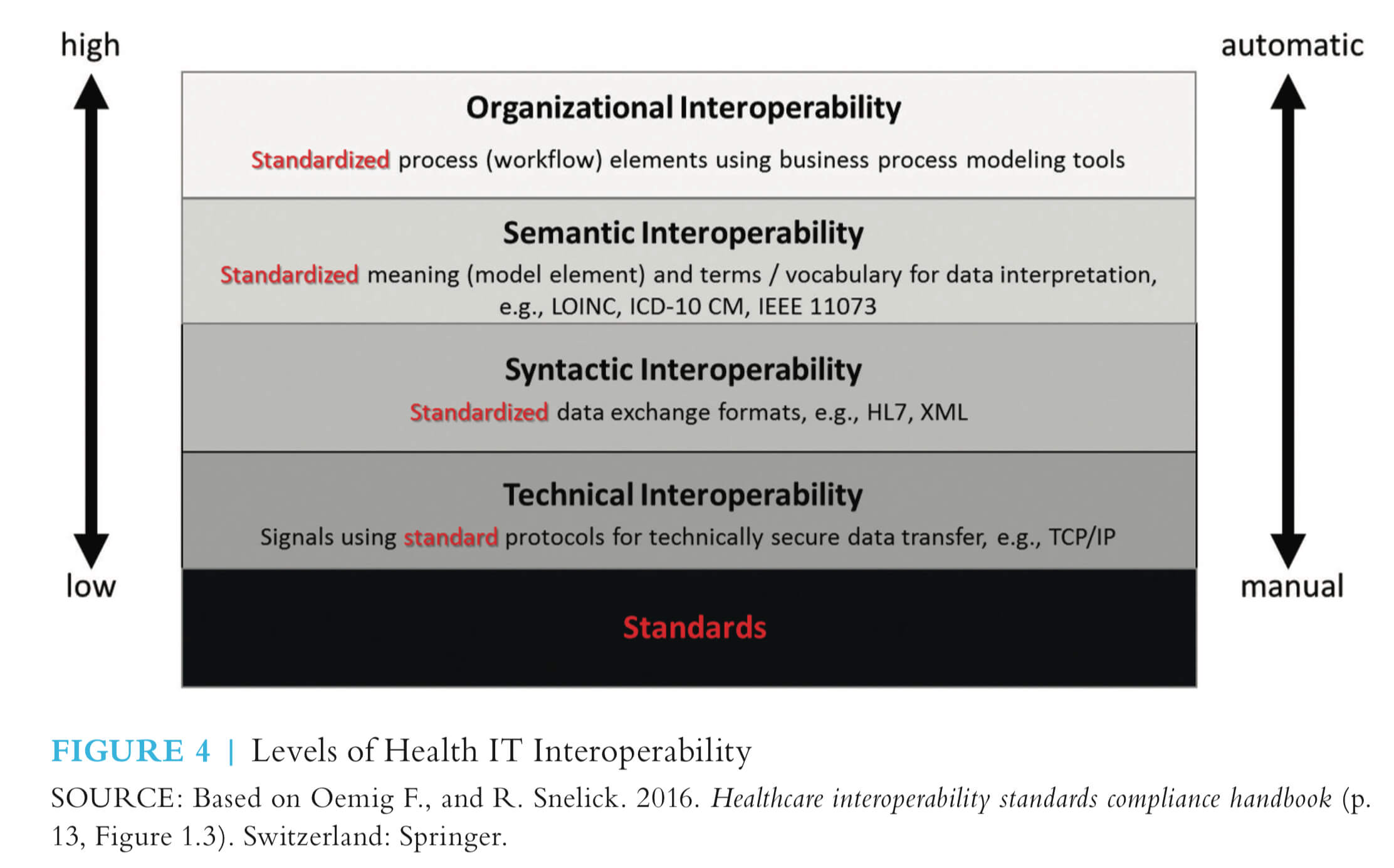
“True interoperability is the ability to seamlessly and automatically deliver data when and where it is needed under a trusted network without political, technical, or financial blocking.”
In the moment of clinical decision-making, it is critical to have access to all the information needed to make the right decision at the right time for the right person.
The challenge for senior leaders and enterprise architects is to create and foster a vision of interoperability that is not based upon everyone using a single homogeneous system but rather upon having data portability and sharing that enables patients to receive care over time across a continuum.
I have worked in healthcare for almost 40 years in various environments: payer, long-term care, physician offices, home infusion therapy, delivery systems, innovative startups, and large IDNs. Patients and members move through systems and providers because of changes in insurance, geography, job changes, physician retirement, or simple proximity and access. This is defined as Macro-level integration and is performed by lab providers, HIEs, or other system-to-system integrations. However, as I’ve had conversations with healthcare systems across the country, many organizations are receiving and sending thousands to tens of thousands of faxes every day to share patient information across disparate healthcare systems. Data integration, risk models, and coordinating care is very difficult to perform without stronger macro-level integration.
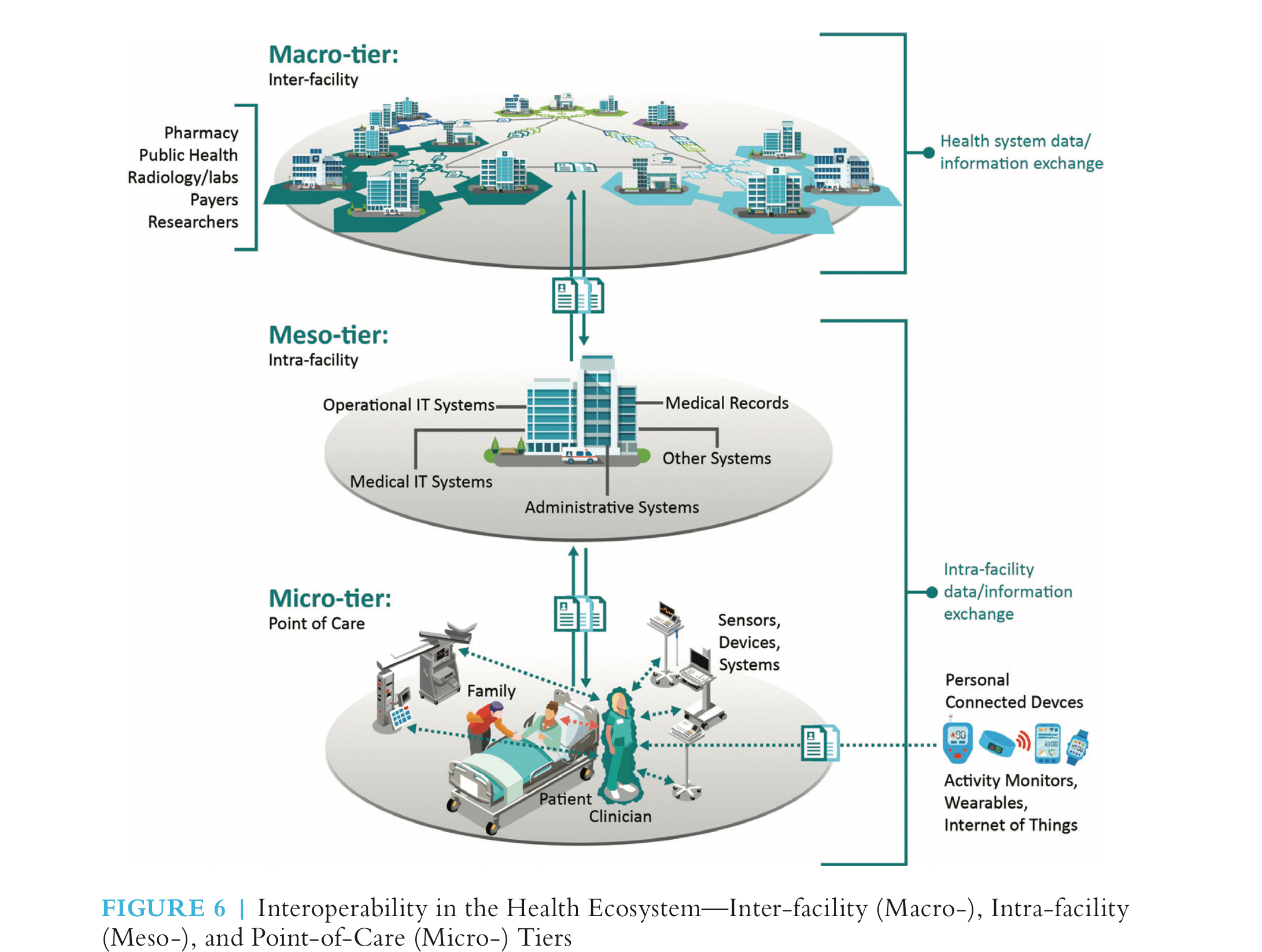
An interesting contribution of this document from NAM is the movement from Macro-tier community data sharing to Meso-tier within a system to Micro-tier at the point of care. Vervint is working on IoT initiatives with healthcare product companies that will impact the micro-tier integration, but what I constantly want to challenge our teams working in this space (and our customers) is how we will address integration at the higher-tiers and into the EHRs and provider workflows.
We are still far from the standards and ability to integrate up and down the stack, across the community, for the life of the patient. But the NAM has given great guidance and should be required reading for anyone procuring or building Healthcare IT solutions.
Here’s a direct link to download the report: https://nam.edu/procuring-interoperability-achieving-high-quality-connected-and-person-centered-care/
Let me know what you think. I want to find a health system interested in doing this — for the sake of our patients.
It won’t happen unless we do it.
